
Editor’s Note: Prakash Menon is the CEO at Basehealth, a science and technology leader that adds genomic precision to predictive analytics and population health management.
Let’s not bury the lead. It’s finally possible to effectively model diseases and predict risk, based on an individual’s unique clinical, lifestyle, environmental and genetic data. True predictive analytics for healthcare have arrived at long last.
Back to The Future
Historical medical information that resides in claims data, electronic medical records (EMRs), and elsewhere has enduring value, but that data remains, by definition, anchored in the past. EMRs, for example, give us a much better view of what happened than what is happening now or what will happen next.
Today, faster diagnostics, machine learning on large sets of data and nascent proteomics (among other things) promise a real-time understanding of health.
What’s trending? What events signal anomalies? Which are good surrogates for something else? Where are there strong and weak correlations population-wide? Just understanding what’s going on in the present tense is a big deal.
But the most exciting frontier in healthcare and population health is the future. This is what we’ve all been talking about, for what seems like, ages. I hope articles about this subject have been popping up in your email feeds as frequently as they have in mine. The time is now: 2016 will be the year of predictive analytics.
Why? The excitement is based on how predictive analytics have proven – in small-scale pilots – to decrease costs, more effectively direct care, better inform underwriting and swiftly re-orient our system towards proactive, preventive disease management.
That famous William Gibson quote is especially appropriate here: “the future is already here, it’s just not evenly distributed.” Soon, predictive analytics will be prevalent, not merely promising.
It Starts With Precision
In addition to outlining what will take us from early adoption to an early majority in terms of predictive analytics, I also hope to clarify a few buzzwords along the way.
Almost a year ago at the 2015 State of the Union address, President Barack Obama spoke of funding a National Precision Medicine Initiative, catapulting that new term into the limelight:
“We must gain better insights into the biological, environmental and behavioral influences on [chronic] diseases to make a difference for the millions of Americans who suffer from them. Precision medicine is an emerging approach for treatment and prevention that takes into account individual variability in genes, environment and lifestyle for each person.”
While definitions of precision medicine vary, one thing is generally agreed upon: precision medicine is about being able to classify people precisely, based on their susceptibility, their microbiology and/or their prognosis, at a considerably higher resolution than ever before.
As the National Research Council has explained, “preventive or therapeutic interventions can then be concentrated on those who will benefit” (my emphasis).
So, what exactly is the relationship between precision medicine and predictive analytics? How do we get from personalizing care at the individual level to intervening preventatively, based on things we understand to be of very high likelihood? This is a distinction that muddies the water for many in our industry.
Allow me this: whole genome sequencing and health data analysis provide perspectives most useful when put to work predicting the future. It’s one thing to see precisely right in front of you. It’s yet another to peer around the corner.
If extrapolating based on initial conditions is the game, then higher-resolution conditions will provide higher-quality output. Precision medicine makes true predictive analytics possible. One is a requirement for the other.
But Context Is Ultimately King
Certainly, in narrow use cases, acute care and rare disease states, precision itself and alone can be life-changing. It’s important to acknowledge that.
Each year, seven out of 10 Americans die from chronic diseases. The vast majority of America’s healthcare costs are associated with chronic health issues and conditions that we can, in fact, prevent if we can just manage to give patients and providers advance notice.
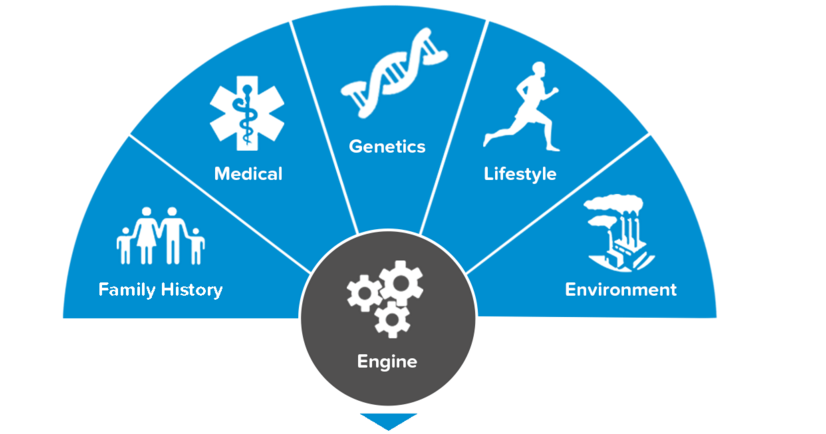
To give advance notice, we need the data upon which to compute these insights. We certainly need the level of precision genomics provides, but we also need every bit of surrounding context too. To affect broad systemic change, we need a wide purview.
What we’re seeing in the field is that the explosion of information available to us not only from the human genome, classic labs and family history, but also from a comprehensive assessment of lifestyle, environmental, dietary and activity data that makes true predictive medicine a “right now” opportunity, and not just the stuff of science fiction.
Which is all to say: prediction requires precision, but it does not require precision alone. Predictiveness comes from a simultaneously wide and narrow aperture. You need a lot of data, but you need high-accuracy tent-poles too.
In a recent whitepaper, Optum similarly argued that today is the tipping point for predictive analytics in healthcare because the data we now have at our fingertips makes much higher-reliability outputs possible:
“Predictive analytics uses regression models on underlying data to predict outcomes. This [fact] is not new to healthcare. The challenge, in past years, has been the underlying data.
[For example], claims data alone does not get at a patient’s overall health or disease-specific functioning. This clinical data is often handwritten, dictated or incomplete. Hence, predictive modeling [historically] relied on relatively small data sets, often of poor quality, and with limited variables. The result was marginally predictive models.”
In other words, the actual pragmatics of making predictions isn’t rocket science; what’s been holding us back is that we’re only as good as the data that we draw upon. We now finally have the raw materials necessary to project into the future with accuracy.
Why Should I Care?
Here are a few of the business cases. These are the carrots.
These new capabilities can realistically help everyone from administrators modeling things like hospital admissions (and readmissions) to providers understanding things like the likelihood a patient will develop congestive heart failure to risk-bearing organizations like ACOs doing things like proactively identifying gaps in care, not to mention payers who wish to proactively and progressively drive down risk by investing in population wellness.
But the market inevitability of healthcare’s Triple Aim (background here), which is supported by the NIH, Medicare, Medicaid and many others, mandates that we simultaneously pursue better care, better health and lower costs. Those are the sticks. Those are the structural drivers, and they are emphatic.
