The outcome of the recent election caught many people, and many forecasters, by surprise. How could their predictions have missed the mark so significantly? Granted, there were a number of people who predicted the outcome more accurately, but many of those who used data models to analyze the likely outcome are left now with head-scratching and postmortem analysis in order to improve their methods.In their book Superforecasting, The Art and Science of Prediction, authors Philip Telock and Dan
Read More
Can Artificial Intelligence Reduce “Notification Overload” for Clinicians?
One of the unintended consequences of moving healthcare onto EHRs has been an increase in time spent reviewing a much-increased volume of messages for the clinician. EHRs were supposed to simplify and streamline the in-office and in-hospital workflows, but what has happened instead has been “notification overload.” A recent article published in JAMA showed that, for primary care physicians, managing EHR notifications costs about an extra hour of work per day. In a fee-for-service environment,
Read More
Can AI Reduce The Prior Authorization Burden in Healthcare?
One of the most frustrating elements of the current healthcare environment is the administrative burden of prior authorizations for medications and procedures. It is a frustration for providers, for patients, and for payers. Is there any way to solve this dilemma?For physicians, an estimated 20 hours per week is spent in prior authorization activities, costing an average of $83,000 in excess annual overhead per physician. Is there an actual benefit for this effort? Most physicians say that
Read More
Can Artificial Intelligence Improve Patient Engagement?
A recent article in The Commonwealth Fund blog, “Envisioning a Digital Health Advisor,” raises the question of being able to use smartphone apps to get real-time, accurate and personalized guidance for health concerns. While one can envision the convenience, affordability and peace of mind that would result from their use, such services face a number of hurdles before they become reality. As a result, the “digital revolution” has not yet greatly affected most people’s interactions with the
Read More
Why Do We Need A New Operating System for Effective Shared Care Plans?
The way we pay for healthcare is changing. The transition from fee-for-service (“fee for volume”) to value-based care is beginning to take shape, and will do so increasingly in the next few years. Federal pressures as well as private industry pressures are driving this change, as reviewed nicely in a white paper by Houlihan Lokey, “Value-Based Care.” But do we have the right tools? Value-based care implies that health care delivery be coordinated across all the different settings of care that
Read More
Why Shared Care Plans Is the Future of Care Coordination
A recent study of healthcare organizations showed that most are not prepared to deliver standardized longitudinal care across multiple provider systems. Shared care plans will be the centerpiece of coordinated care delivery, incentivized by the move from fee-for-service to value-based care. In 2015, Medicare unveiled its plan to transition to quality-based payments via the Merit-Based Incentive Payment System (MIPS), which will sunset and subsume earlier quality-encouraging programs, and move
Read More
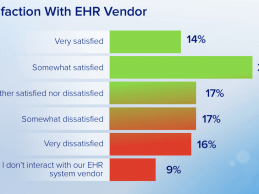
Why I Despise my EHR, But I’m Still Using It
Modern electronic health records (EHRs) have become the norm in U.S. health care — nearly 80 percent of office-based physicians use them, up from 40 percent in 2009, according to federal data. But while adoption is up, satisfaction has plummeted. In 2010, about 61 percent of physicians liked their EHRs (were satisfied or very satisfied, according to periodic AMA surveys). This dropped to 48 percent in 2012, and in 2014 satisfaction rates were only 34%. Physicians have come to
Read More
New Paradigm: An Operating System for Value Based Care
Health care in the U.S. is on the threshold of fundamental change. Powered by advances in federal policy, the underlying way in which we pay for health care is moving from the traditional fee-for-service, pay-for-volume historic approach to one that pays for demonstrated value. The way in which value is measured is still evolving, but risk-sharing, measuring the health status of populations, and coordinating care in order to improve effectiveness and reduce the total cost of care are the basic
Read More
Is Universal Health Data Platforms the “Holy Grail” of Interoperability?
Health information exchange (the verb) has been the goal of health IT, now that we have moved into the “post-EHR adoption” era of healthcare. Published and private surveys have shown that about 80% of physician practices have implemented an EHR, and of those, about 90% have participated in meaningful use. The challenge before us now, then, is somehow connecting the fragmented places where health data resides, and bring them together into a unified health data layer that is current,
Read More
The Critical Role of Health IT in the Ebola Outbreak
A recent article by Atul Gawande in The New Yorker describes the level of preparedness at Texas Health Presbyterian Hospital in Dallas, as it encountered the first case of Ebola to be diagnosed in the U.S. The emergency department was as prepared as anyplace, and had rehearsed the scenarios, and reviewed the CDC checklist for Ebola preparedness. They had asked about fever in people who had traveled from the region of West Africa beset by Ebola, per the protocol. In fact, the triage nurse in the
Read More