What You Should Know:
– Innovaccer is unveiling six new breakthrough solutions that help providers accelerate their success with population health, consumerism, and value-based care.
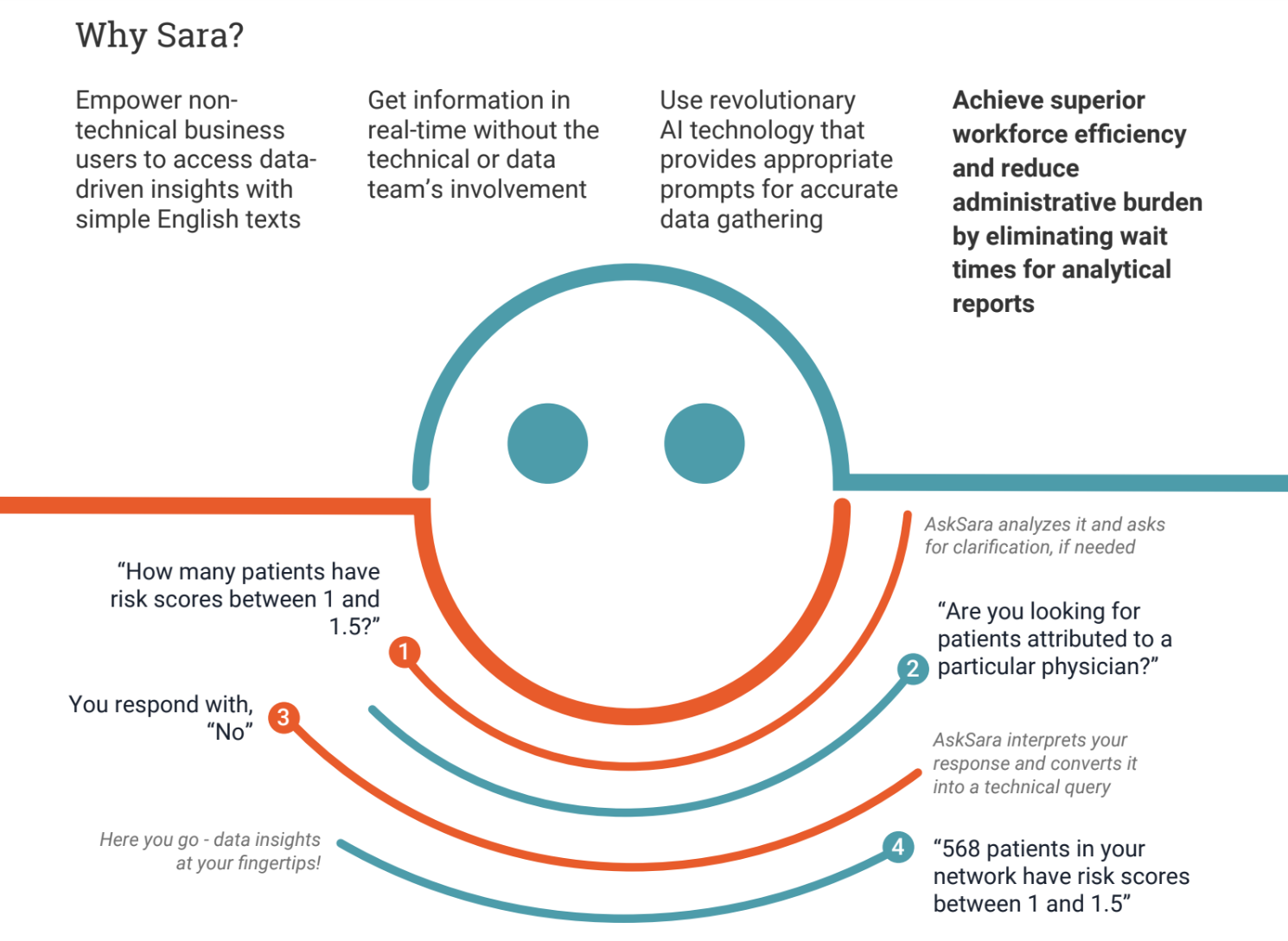
– Leading the lineup is Sara, the first conversational AI for healthcare analytics. Sara is a conversational AI assistant that literally puts the full breadth and depth of enterprise healthcare analytics into the hands of healthcare managers, physicians, and care teams. Anyone can ask Sara complex questions about their health system’s population and get immediate answers on clinical, financial, or operational metrics.
The other five new solutions include:
Innovaccer’s Health 1:1 is the first enterprise customer relationship management (CRM) solution built exclusively for healthcare. By integrating all clinical and consumer data for a patient into a longitudinal consumer/patient record, health systems can find new patients, guide their care, and retain them for life.The integrated data also helps to tie financial outcomes to patient acquisition and retention initiatives, documenting downstream ROI. As the industry’s only Enterprise CRM that’s populated with all of your relevant consumer and patient data from day one, there’s no faster or more effective way to accelerate your success with consumer and patient engagement.
Innovaccer’s Health Equity is a comprehensive solution that helps health systems improve service delivery to underserved communities. They can use Area Deprivation Index (ADI) and member-level Social Vulnerability Index (SVI) scores to estimate socioeconomic needs, build cohorts based on social risk, develop targeted interventions to close care gaps and tap the largest network of community resources for referrals. Social Determinants of Health (SDoH) insights integrated into clinical workflows help providers close care gaps at the point of care. Assessments and surveys capture a population’s complex and changing social needs, while automated workflows drive collaboration among patients, providers, and community resources with closed-loop confidential communications. And health leaders can track performance to measure and improve their health equity strategy using the solution’s customizable dashboard.
Innovaccer’s Network Optimizer is a one-stop solution for healthcare leaders to visualize market dynamics and use data to improve network design, optimize network performance, manage referral steerage, reduce network leakage, decrease care costs, and improve care quality. It uses multi-market, all-payer claims data to simulate network configurations and their influence on network performance with predictive analytics. Network Optimizer also helps predict and preempt the impact of inclusions/exclusions of any given provider group on the health system’s performance across network characteristics such as quality score, adequacy, utilization, and more.
Innovaccer’s Readmission Predict helps providers optimize discharge care planning and care management by using AI to predict the likelihood of readmissions at the time of discharge. Readmission Predict also analyzes Admission-Discharge Transfer (ADT) feeds, claims profiles, and SDoH data to suggest targeted interventions providers can act on. Care managers can then prioritize resources and devote additional appropriate attention to at-risk patients to improve care outcomes, helping avoid readmissions and associated costs.
Innovaccer’s Risk AI boosts coding accuracy by analyzing unstructured EHR and clinical data to help providers identify suspect codes and close coding gaps at the point of care. It uses AI, ML, and NLP to analyze years of unstructured documents—such as patient charts, progress notes, and discharge summaries—to flag potential conditions that might impact a person’s risk score. Suspect codes for these conditions are shown to physicians within their EHR clinical workflow, where they can easily view, accept, or reject them during the clinical encounter, closing appropriate coding gaps at the point of care. This cuts coding time, enhances coding accuracy, improves physician satisfaction and efficiency, and maximizes risk contract outcomes by significantly refining population stratification.
