What You Should Know:
– Health equity – or the lack thereof – is one of the biggest challenges facing US healthcare organizations today.
– A new report from Accenture, US health inequity: beyond the statistics, analyzes the role US healthcare ecosystem participants can play in addressing health inequities due to race and ethnicity. The statistics are staggering.
Analysing Key Trends Concerning Health Inequities
To understand the human and economic impacts of health inequity, Accenture conducted a systematic analysis of peer-reviewed literature and critical opinion leader views to then collate insights from extensive client engagements.Additionally, Accenture spoke with subject matter experts from the life sciences, healthcare and public health industries. Through these actions, one could synthesise health inequities’ leading causes and effects.
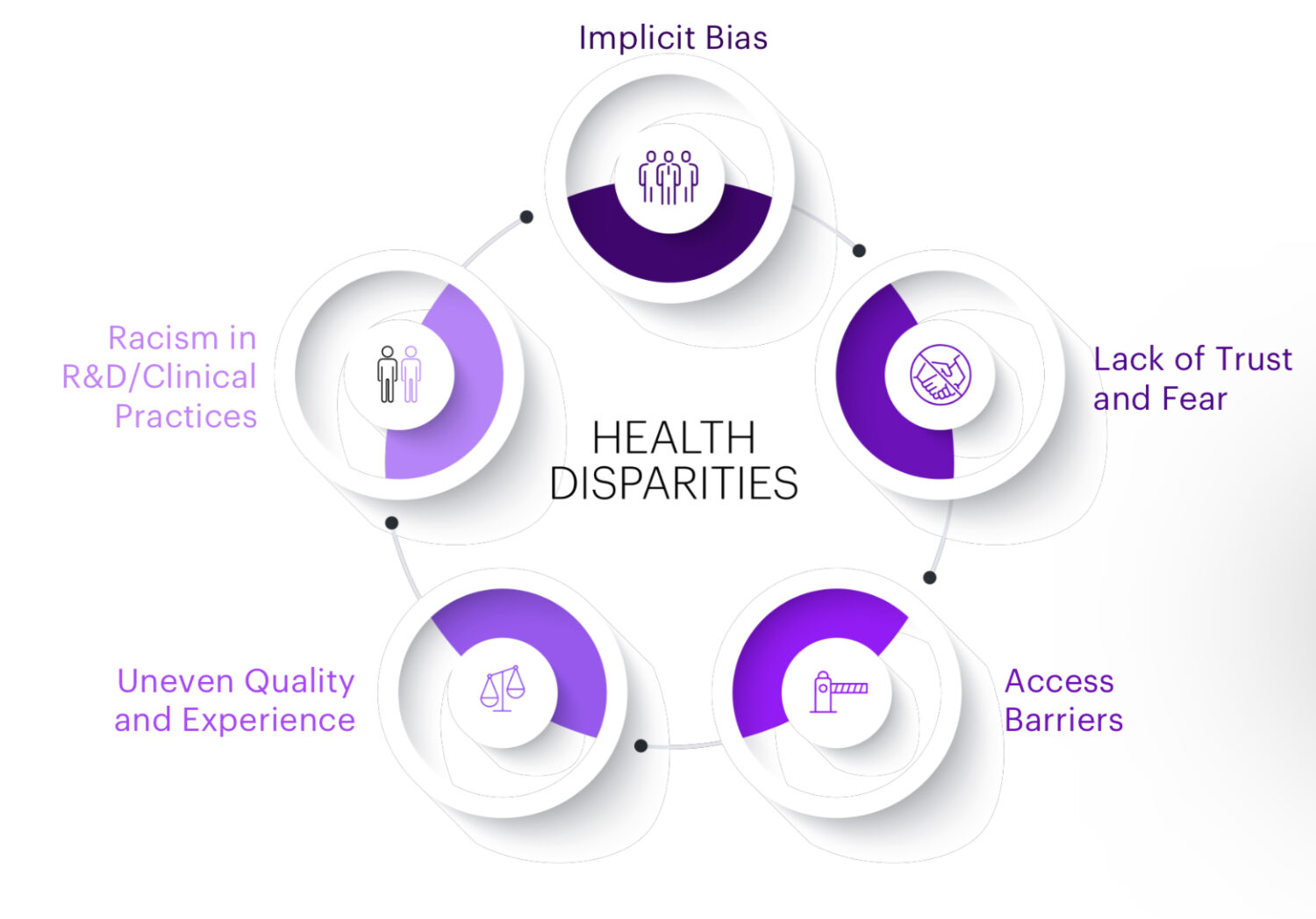
Accenture identified five interconnected areas that negatively affect people:
1. Implicit bias: Implicit racial and ethnic biases are unconscious attitudes or stereotypes that affect our understanding of, and responses to, individuals and groups other than our own. These biases erode quality of care and access for underrepresented patients, in turn leading to a lack of trust in, and even fear of, the healthcare system as well as lowering participation by POC in their healthcare journey.
2. Lack of trust and fear: Given longstanding issues with the medical system (such as mistreatment of, and unethical studies among POC in the US), their relationship with the healthcare system is characterized by a general lack of trust and high levels of fear.
3. Access barriers: Access barriers are roadblocks which prevent underrepresented groups from receiving equal access to care such as the affordability of care/medicines, the effects of implicit biases, health education, participation in clinical trials and other barriers such as language or transportation.
4. Uneven quality and experience: Stark differences in the quality of care exist between races. Patients from racial and ethnic minorities frequently receive sub-par care and experience worse outcomes relative to white patients. This uneven quality is directly tied to biases, trust and fear, and access barriers.
5. Racism in R&D/Clinical practices: Lack of representation of people of color (POC) among both patients and physicians, barriers to access and other obstacles like bias, lack of trust and fear, and limited care access all limit the quality of health and research outcomes among affected groups.
According to the report, health ecosystem players’ current efforts to address inequities are disconnected from the daily realities faced by underrepresented communities. Their efforts need to be more relevant, organized, streamlined and cohesive. To achieve health equity, the next generation of actions must consider three core areas that tackle the five key interconnected areas:
1. Mitigate bias in data analytics and algorithms: Clinical algorithms are at the heart of the digital core of Health organizations. They intend to improve accuracy and efficiency but have sometimes proven to widen healthcare disparities. The most cited example is the large commercial health decision algorithm that used healthcare costs as a proxy for health needs, which inappropriately led to Black and African American patients being labeled as “healthier” than equally sick white patients. To advance health equity, data analytics and algorithms must be inclusive, fair, accountable, transparent and easily explainable.
2. Design inclusive products and services: Health equity must be considered from the start of product and service design. Inclusive design methods enable and draw on the full spectrum of human diversity and individual experiences to create solutions. This does not mean that a single product or solution meets every person’s needs. Instead, it means designing different ways for people to receive the same access, experience and outcomes while having a sense of belonging. Considering health equity at this stage encourages better practices, greater accessibility and a more inclusive healthcare environment which drives value for people and ecosystem participants.
3. Create sustainable structural change: To make long-lasting, meaningful change, participants must ensure that their actions bring about structural change. Racism and implicit biases are embedded throughout the ecosystem. Addressing institutional policies such as inclusive hiring practices, the types of partnerships created, and how participants execute clinical treatment and tools will have far- reaching effects on the sustainability of the healthcare ecosystem. Additionally, engraining equity as a core tenant of participants’ foundation will aid in normalizing these activities across the ecosystem.
Lastly, the report includes suggested actions for healthcare payers and providers, along with suggested actions for bio Pharma companies and public health institutions, to mitigate healthcare inequities, as follows:
Mitigating bias in data analytics and algorithms(healthcare payers and providers)
1. Employ critical evaluation when using non-user-generated demographic data: Analyze gaps in data collection and work with local community brokers (like EMTs, social care organizations, food pantries or schools) to inform available public (or purchased) datasets. This will produce more inclusive data around disease onset, hospitalization and adherence to treatment plans. Comprehensive demographic data collection is a health equity priority for CMS.
2. Leverage existing member health processes and outcomes: Stratify them by race, ethnicity and language (REL), sexual orientation and gender identity (SOGI), disability status, rurality and other variables. Acknowledge bias and gaps in data analysis that don’t accurately reflect communities.
3. Implement frequent and standardised audits: Assess algorithmic and data collection processes. Use machine learning auditing techniques to build in representational fairness, counterfactual reasoning, error rate balance and error analysis to account for confounding racial/socioeconomic factors.
Mitigating bias in data analytics and algorithms(biopharma companies)
1. Develop equitable algorithms: Set organisational diversity standards for any data leveraged for any R&D or other algorithmic purposes to ensure that data is more representative and less fragmented. Doing so will also streamline the ability to amalgamate this data for additional analyses on both social and clinical dimensions. Assess algorithms for bias potential/relative degree of inherent bias. Continuously revise algorithms as more diverse data sets become available. Develop non-biased diagnostic algorithms. Also, consider Institutional Review Board-type data auditing boards or 3rd party auditing of data and algorithms to identify risks and bias.
Mitigating bias in data analytics and algorithms (public health institutions)
1. Use data and analytics to enhance decision-making processes: Create public health dashboards that are broadly accessible and communicate metrics stratified by race, ethnicity, gender and geography, focusing on reporting disparities. Invest in automated data capture and reporting that can produce closer to real-time insights to reduce process hurdles and increase the uptake of evidence-based programs by underrepresented communities.
2. Convene ecosystem partners to advance interoperability, such as enhancing the infrastructure for health information advances: Promote data sharing, interoperability and cross-agency/organization partnerships to be more effective in implementing and adopting programs and interventions.
Ensuring inclusive product and service design (healthcare payers and providers)
1. Ensure that cultural competency training, upskilling and credentials are embedded throughout the organization: Help meet cultural needs through third-party partners (e.g., SameSky, Violet Health, Spora Health). Engage community-based organizations and leaders from the beginning. Defer to the community via interviews and keep them engaged in the design experience to create culturally appropriate service designs and facilitate omnichannel care access.
2. Focus on improving the health literacy of members: Create Explanation of Benefits (EOB) guides and claims material simplified at a more accessible reading level with clear, multilingual and culturally tailored content. Payers can also collaborate with third parties that focus on outreach to specific populations (e.g., CityBlock Health).
3. Implement omnichannel engagement strategies: Provide high-tech or analog/lower-fidelity digital alternatives for people to choose from. Providers can co-design experiences with trusted community leaders (like faith leaders, teachers, librarians and EMTs) using community networks for patients through sustainable partnerships with community-based organizations.
Ensuring inclusive product and service design (biopharma companies)
1. Incorporate health equity considerations in early development and at launch planning: Organize a cross-functional team with individuals who represent specific patient populations by demographic, geography, or living conditions. Tailor marketing plans and materials to include diverse perspectives from the voice of the customer research to appropriately reach the target patient population and respective healthcare professionals.
2. Enhance the patient experience across their entire journey: Involve diverse patients and caregivers (across dimensions of age, race, socio- economic status, ability, etc.) in the design of the clinical trial protocol and associated planned experience. Incorporate more holistic segmentation and design mindsets to provide products and services tailored to specific communities thereby extending these thoughtful strategies across more disease states. Engage relevant partners (e.g., community-based, systems-based) to create patient support programs that drive care coordination beyond financial aspects, such as emotional support, transportation, etc.
Ensuring inclusive product and service design (public health institutions)
1. Develop health and life intervention: Develop and implement interventions to sustainably improve underrepresented groups’ health and overall life outcomes. This may also be done through collaborations, such as public-private and community partnerships, providing ridesharing to help with transportation barriers or leveraging funding tools, like state waivers, to approve broader use of Medicaid dollars for social services related to housing, food insecurity, transportation and interpersonal violence.
2. Influence health equity accountability: Use contractual agreements to hold key partners responsible for health equity. For example, state contracts with managed care organizations (MCOs) can ensure accountability for health equity goals and build momentum. States can also increase the emphasis on outcomes-based care as well as support and review to key partners to ensure a health equity lens is being applied at each step of the decision-making process.
Creating sustainable structural change (healthcare payers and providers)
1. Reinvent care delivery: New care delivery models must tie to payment innovation and address patient access and quality needs. Rising patient demand combined with decreasing provider supply will ultimately harm the most vulnerable among us. Health systems need to stabilize the existing workforce, source talent more flexibly, deploy top of license clinicians more effectively (focusing on what they trained to do) and reskill their teams
2. Move from unsustainable one-time philanthropic efforts to scaled social investments: These social investments aim to improve social, economic, and environmental conditions in vulnerable communities while simultaneously creating opportunities for financial returns for investors. These programs, such as Kaiser Permanente’s Thriving Communities Fund, address inequities at the root, generate value for the entire health system and empower underserved communities.
3. Align executive incentives to reducing disparities: Actions such as tying portions of annual executive bonuses to their success in reducing disparities create greater urgency, generate innovative and cross- functional solutions and prioritize health disparity initiatives. These incentives also create a trickle-down effect and permeate the rest of the company’s culture as leadership emphasizes these actions (e.g., SCAN Health Plan)
4. Develop care continuum plans that integrate clinical research: Every patient should have the opportunity to be matched to the best therapy for their personal situation, and that includes clinical research. In addition to clinical research improving adherence rates, underrepresented communities can access previously unavailable therapies.
Creating sustainable structural change (biopharma companies)
1. Ensure everyone can afford and access the latest medicines: Engage in innovative access models—pricing, distribution and contracting—that drive equity in access and reduce affordability barriers and further offset barriers for underrepresented communities through patient assistance programs, bridge programs, free trial offers and co-pay programs. Create new channels for access to services or treatments. Focus especially where communities of color are disproportionately impacted by lack of proximity to care for therapies that require access to a center of excellence (CoE) or academic center’s care. Ensure that access models drive equitable and broad access and that people from different demographic groups know, can access, and use these support programs.
2. Improve clinical trial diversity through multiple actions: Partner with non-traditional organizations such as retail pharmacies and local labs that are entering the clinical trial space to identify trial-ready, diverse patient populations quickly. Consider decentralized and hybrid clinical research methods to lower the barriers to entry that many marginalized communities face when accessing clinical trials. Develop diversity standards to ensure equal representation among investigators. Provide greater optionality for ways patients might engage with clinical trials in certain parts of the protocol. Identify target patient populations based on disease epidemiology and any social determinants of health that exasperate health status.
Creating sustainable structural change (public health institutions)
1. Implement more proactive public and institutional policies: Intentionally think about how underrepresented communities would fare and benefit when advancing regulatory actions, rulemaking, and other policy levers. Analyze past performance of decision impacts on disparate areas beyond health, from labor to demand for social services as part of policy formulation process. Include social risk factors such as dual eligibility, low-income and rural residency as variables in the payment structure so that providers who disproportionately treat these patients are not penalized due to worse outcomes.
2. Create key partnerships across the entire healthcare ecosystem: Create and lead interdisciplinary alliances that address the social determinants of health while including community members and leaders in these coalitions. Payers, providers, and community groups could better drive referral networks and organize tailored interventions if they worked together. Invest in and develop early- stage community-based organizations. Support the growth of early-stage organizations by connecting them with needed resources (e.g., government funding, infrastructure, technology tools).
